March 16, 2022
The Consolidated Appropriations Act of 2021 (CAA) was signed into law by Congress in December 2020 to provide greater transparency about what medical costs a health plan’s members are responsible for paying. This legislation is also known as the “No Surprises Act.”
Independence Blue Cross (Independence) welcomed this guidance because transparency is an essential part of our relationship with our members.
The No Surprises Act requires certain things to be spelled out more clearly on members’ ID cards. In compliance with this requirement, our members are receiving new member ID cards. I’d like to give you a quick tour of these features and how useful they can be.
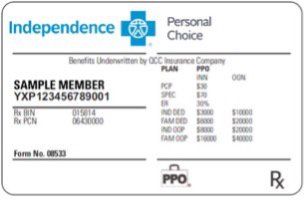
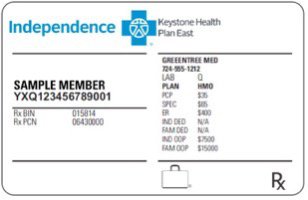
If you’re an Independence member, the information that appears on your member ID card varies depending on what type of health plan you’re enrolled in (e.g., HMO or PPO). I’ll explain those differences in a moment. But first I’d like to point out some of the terms you might see on your ID card and what they mean.
• Primary care physician (PCP): The doctor who will treat your general health needs and coordinate your care.
• Specialist (SPEC): A doctor who practices in one area of medicine, such as a cardiologist (heart doctor).
• Emergency room (ER): Where you should go in a medical emergency — a situation where your medical or mental health symptoms are so severe that your health may be in serious jeopardy if you don’t get immediate medical attention.
• In-network (INN) and out-of-network (OON) deductibles (if applicable to you): The amount you pay each year for covered health care services before your health plan starts to share the costs. If you don’t have a deductible, you will see “N/A.”
• Out-of-pocket (OOP) maximums: The maximum amount you will pay for covered health care services each year, not including your monthly premium.
A Preferred Provider Organization (PPO) plan allows you to see health care professionals both in and out of network, though you will typically pay less in network. If you have a PPO plan, your member ID card will spell out what you would pay in network versus out of network.
It will also explain what your individual (IND) and family (FAM) in- and out-of-network deductibles (DED) and maximum out-of-pocket (OOP) costs are.
A Health Maintenance Organization (HMO) plan requires you to use in-network health care providers and emergency rooms. If you have an HMO plan, your ID card will explain your copays for PCPs, specialists, and ER visits. It will also show your individual and family deductibles and maximum out-of-pocket costs.
A high-deductible health plan (HDHP) has lower premiums, but it has higher deductibles you must meet before your health plan will begin to pay your health care expenses. If you have an HDHP, your ID card will show what your individual and family deductibles are as well as your individual and family maximum out-of-pocket costs.
There may be times when you may need to access your member ID card digitally. For instance, it may be helpful if you don’t have your physical ID card on hand because you left it at home or lost it, or if you need to fax or email it to a health care provider. Here are some easy ways to do this:
When you log into your member account at ibx.com, you’ll see your digital member ID card right on your home page. You’ll have the option to print the card or save it as a PDF; email or fax a copy of the ID card; or order a replacement ID card. If you have dependents on your health plan, you’ll be able to do the same with each dependent’s ID card. If you haven’t yet created your member account, visit ibx.com and sign up today.
You can download the Independence Blue Cross mobile app on your iPhone or Android smartphone, and log in using the same username and password you use for your member account at ibx.com. You’ll see your digital member ID card right on your home screen.
You’ll have the ability to email or fax the card or order a replacement, both for yourself and for any dependents who are on your health plan. If you have an iPhone, you can also select Add to Apple Wallet to make your ID card easily accessible.
Independence appreciates our members and the opportunity to help them take care of their health.
This content was originally published on IBX Insights.
Paula Sunshine is senior vice president and chief marketing executive at Independence Blue Cross. She oversees all commercial and consumer marketing activities, including digital assets such as ibx.com and the IBX mobile app. Ms. Sunshine earned a bachelor of arts degree in mathematics from Emory University and a master of business administration from the Wharton School at the University of Pennsylvania.